Poison Statistics National Data 2016
Reports to U.S. Poison Control Centers
How Many?
In 2016, the 55 U.S. poison control centers provided telephone guidance for nearly 2.159 million human poison exposures.1 That’s about:
- 6.6 poison exposures/1000 population,
- 41.3 poison exposures in children younger than 6 years/1000 children,
- 1 poison exposure reported to U.S. poison control centers every 14.6 seconds.
| Year: 2016 | |
| Human Poison Exposures | 2,159,032 |
| Animal Poison Exposures | 54,019 |
| Confirmed Non-Exposures | 6,776 |
| Info Calls - Drug ID | 137,880 |
| Info Calls - Other | 352,335 |
| Total | 2,710,042 |
What Ages are Affected?
While young children (younger than 6 years) comprise a disproportionate percentage of the cases, poisoning affects ALL age groups, from infants to seniors. Peak poisoning frequency occurs in one and two year olds, but poisonings in teens and adults are more serious. Notice that the greater proportion of males in poison exposures occurring in children younger than 13 years switches to a female predominance in teens and adults.
 |
Across all ages, there were 660 poison exposures reported per 100,000 population. The highest incidence occurred in one and two year olds (8,083 and 7,675 exposures/100,000 children in the respective age groups). For ages 50 years or older, 256 exposures were reported per 100,000 population.1
 |
Children younger than 6 years comprise nearly half of poison exposures (46.4%), followed by adults (39.0%), then teens (7.7%).
 |
Why?
Across all ages, 77.8% of poison exposures reported to U.S. poison centers in 2016 were unintentional, 18.1% were intentional, and 2.5% were adverse reactions. In children younger than 6 years, 99.4% of exposures are unintentional, compared to only 33.8% of teen exposures and 59.7% of adult exposures.
 |
Most Common Substances Implicated in Poison Exposures?
Cosmetics and personal care products lead the list of the most common substances implicated in pediatric exposures (children younger than 6 years, NPDS, 2016). Cleaning substances and pain medications follow. These exposures are nearly always unintentional.

Pain medications lead the list of the most common substances implicated in adult poison exposures (20 years old or older, NPDS, 2016). Sedatives and sleeping medications, antidepressants, and cardiovascular medications follow. These exposures are often intentional.

Most Serious Poisonings?
Frequency statistics are only a part of the poisoning story. To determine where to focus prevention efforts, we also need to know which poisonings are serious.
Fumes/gases/vapors are the single most frequent cause of pediatric fatalities reported to Poison Control. The table below shows poisoning fatalities in children younger than 6 years reported to US Poison Control from 2012 through 2016.

The substance categories with the largest number of deaths across all ages (and including intentional exposures) include sedatives and sleeping medications, opioids, stimulants and street drugs, and alcohols (NPDS, 2016).
How serious are poison exposures?
In 2016, 85% of poison exposures reported to U.S. poison centers were nontoxic, minimally toxic, or had at most a minor effect.(Includes the National Poison Data System codes: no effect; minor effect; not followed, nontoxic; and not followed, minimally toxic.)
 |
Intentional exposures were significantly more serious, with a 31-fold greater percentage of serious outcomes (major or fatal effects) compared to unintentional exposures. Of the intentional exposures, 5.28% were major effects or deaths compared to 0.17% of unintentional exposures and 1.24% of all exposures. Just 2.77% of unintentional exposures had a moderate, major or fatal outcome compared to 32.59% of intentional exposures and 8.84% of all exposures.
 |
Exposures in teens and adults were also considerably more serious, with 18.25% of teens and 17.16% of adults having a moderate, major or fatal effect compared to 1.06% of children younger than 6 years. Most exposures in children younger than 6 years (95.85%) were nontoxic, minimally toxic, or had at most a minor effect.
 |
Many poison exposures can be safely observed at home, without an ER visit. Overall, 66.6% of poison exposures were observed without medical intervention in 2016. For poison exposures occurring in children younger than 6 years, 85.1% were only observed at home (without going to an ER or seeing a physician). In contrast, only 47.1% of adults were managed at the exposure site without medical intervention.
 |
These nontoxic or minimally toxic poison exposures that can be safely observed at home are the cases that will most likely be amenable to triage by webPOISONCONTROL®.
Real-time poison exposure data enables surveillance
U.S. poison centers collect data in real time and upload those data every 9.5 minutes (median time to upload). Real-time data are used to find hazardous products quickly, follow substance abuse trends, and detect chem/bioterrorism incidents. Under a grant from the CDC, the American Association of Poison Control Centers and its member poison centers conduct automated, continuous surveillance of poison exposure cases. Alerts are sent when there are an unexpectedly large number of cases in an hour, when there’s an unexpectedly high frequency of a specific symptom, or when there are cases with combinations of clinical effects suggestive of specific poisonings that might require a rapid public health response. Toxicologists promptly investigate these alerts and inform public health officials if outliers are suspicious for events or products of concern.
For more detailed U.S. poison control data, check out the Annual Reports of the American Association of Poison Control Centers:
| 2016 |
2015 |
2014 |
2013 |
2012 |
2011 |
2010 |
2009 |
2008 |
2007 |
2006 |
2005 |
| 2004 |
2003 |
2002 |
2001 |
2000 |
1999 |
1998 |
1997 |
1996 |
1995 |
1994 |
1993 |
| 1992 |
1991 |
1990 |
1989 |
1988 |
1987 |
1986 |
1985 |
1984 |
1983 |
Other U.S. Poisoning Data Sources
According to the CDC, unintentional poisoning is the leading cause of injury death for all age groups.2 It has surpassed motor vehicle traffic fatalities as the leading cause of injury death in the U.S. since 2008.3 Based on provisional counts, 64,070 cases of death due to drug overdose were recorded in the U.S. in 2016.4 The majority of those cases, approximately 66%, involved an opioid.5 This figure, which includes both prescription opioid and heroin use, is five times higher than the number of opioid overdose deaths reported in 1999.5 The continuous rise in prescribing, use, and abuse of opioid drugs and the subsequent increase in opioid related deaths has come to be known as the opioid epidemic. 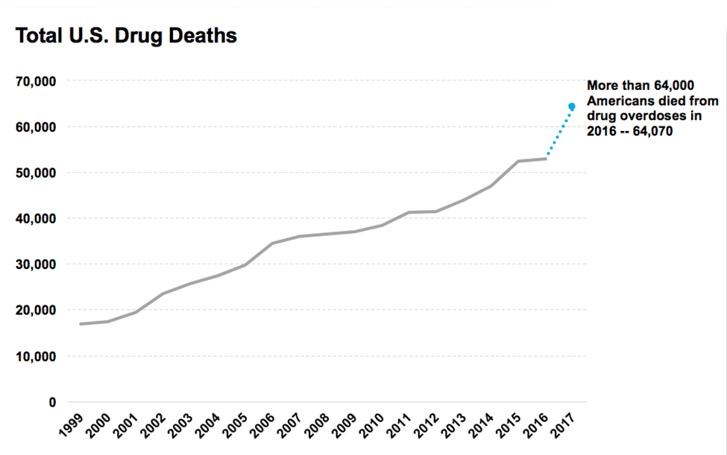 |
The opioid epidemic was initially fueled by the use of prescription opioids like methadone, oxycodone, and hydrocodone. Prescribing patterns for opioid medications followed an upward trend from 2006 to 2012.6 Increased awareness, education, and discussion surrounding opioid use has helped to reign in the prescribing habits of many providers and from 2012-2016, opioid prescription rates declined by 4.9% annually.6
In 2008 it was also reported that the number of deaths involving prescription opioids surpassed the combined number of deaths from both heroin and cocaine use.6 In subsequent years, the number of deaths due to drug overdose, including the number of cases involving opioids, continued to rise. However, by 2015, use of heroin, cocaine, methamphetamines, and synthetic opioids like fentanyl were gaining in popularity. The sharpest rise in drug related fatalities was seen in 2016 and was associated with use of fentanyl and fentanyl analogs with over 20,000 deaths occurring that year.4
 Drugs involved in US overdose deaths,, 2000 to 2016.4 |
The substantial increase in fentanyl deaths has been linked to illicitly manufactured fentanyl that is used to adulterate other drugs of abuse or sold to unsuspecting users under the guise of another drug name.7 The potency of these synthetic opioids can range from approximately 3-10,000 times the strength of morphine by weight and the adulteration of heroin being sold in the U.S. with synthetic opioids has led to alarming medical consequences like naloxone resistance.8
AAPCC Data Disclosure Statement
Related Links
Summary of National Poison Statistics, Reports to US Poison Centers
The Rise of Medicine in the Home: Implications for Today's Children, SafeKids Worldwide, March 2016
Keeping Families Safe Around Medicine, SafeKids Worldwide, March 2014
References
1 Gummin DD, Mowry JB, Spyker DA, Spyker, DA, Brooks DE, Fraser MO, Banner W. 2016 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th annual report. Clin Toxicol 2016; 55(10): 1072-1254. doi:10.1080/15563650.2017.1388-87.
2 10 Leading Causes of Death by Age Group, United States – 2015. National Vital Statistics System, 2 May 2017, www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2015-a.pdf.
3 United States, Congress, National Center for Health Statistics, et al. "Drug Poisoning Deaths in the United States, 1980–2008." Drug Poisoning Deaths in the United States, 1980–2008, U.S. Department Of Health And Human Services, Dec. 2011.
4 Overdose Death Rates. National Institute on Drug Abuse, National Institutes of Health, 15 Sept. 2017, www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
Poisoned? Get Expert Help Online
Don’t guess what you should do. Get accurate answers prepared by poison control experts. This tool will guide you. It’s free. It’s confidential.
Subscribe to The Poison Post®
The Poison Post® is a free, quarterly e-newsletter delivering poison prevention tips right to your inbox!
Support Us
webPOISONCONTROL® is funded entirely through generous private contributions. Your donation to our 501(c)(3) charitable organization will help us maintain and expand this free service so that others can get life-saving help for poison exposures.
