Dig Deeper
The State of Poison Control in the US:
Facing Expanding Demands Despite Budget Cuts
There are currently 55 poison centers serving the U.S.; all 50 states, DC and the territories are served. The first U.S. poison center was established in 1953 in Chicago. There were 17 by 1957, 347 by 1960, 590 by 1970, 641 by 1976, to a peak of 661 in 19781. These early centers were often based in emergency rooms or hospital pharmacies, staffed by ER nurses, residents, hospital pharmacists, or even EMTs - all with no special training in toxicology and limited informational resources and backup. But by the late 1970s, fueled by the Emergency Medical Services Systems Act of 1973, an effort to improve the quality of U.S. poison centers was launched. This effort, dubbed "regionalization" included the development of national standards and accreditation processes for centers.
Those minimal accreditation standards were expensive to implement, leading to a rapid decline in the number of U.S. poison centers - to 384 in 1983, 100 in 1992, and 55 today (2015). The remaining centers served larger and larger regions, and in most cases the decline in numbers that occurred in the 1980s and 1990s led to improved services by increasing the portion of the population served by accredited poison centers. These accredited centers had dedicated health professional staff with certification as poison specialists or board certification in clinical or medical toxicology, 24/7 service, extensive on-site resources, medical toxicologist backup, comprehensive regional poison prevention programs, educational programs for health professionals and poison hazard surveillance efforts. All in all, the accredited regional centers were light years ahead of the small ER-based poison center of the 1970s. They had become concentrated centers of expertise.
While the decline in the number of U.S. poison centers led to better service when it resulted from the elimination of non-accredited centers, over the last two decades the accredited poison centers are increasingly threatened by funding shortfalls. Losing a large accredited poison center risks leaving a segment of the population without poison control services or risks exposing those struggling with a poison emergency to the destabilizing, understaffed and unsafe transition of consolidation. Further, the loss of an accredited center eliminates local health professional training in toxicology; local public education; and toxicologist involvement in research, preparedness, hazard surveillance, public health policy and incident response. This persistent and protracted chipping away at the poison control infrastructure threatens poison control in the U.S. today. Nearly all U.S. poison centers are currently accredited (53 of the 55), but despite the accreditation, most are inadequately funded and face continuing funding battles - serving not just as a distraction, but sometimes actually jeopardizing service.
Cost & Cost Benefit
In 2012, a report issued by the Lewin Group showed that the total cost of providing poison control services in the United States was $136M, with 13% provided by the Federal government (through HRSA), 62% provided by state and local funds, and 25% provided by private funds (host institutions such as hospitals and pharmacy schools, donations, and research grants).2 The report is based on 2011 funding of poison centers and is the most recent compiled national data available. Based on a 3% annual healthcare inflation rate, the cost of providing poison control services in the United States in 2015 is approximately $153M.
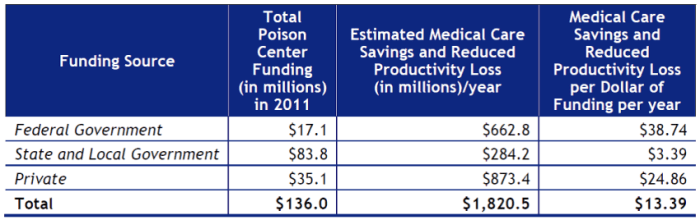
Source: Lewin Group report "The Value of the Poison Center System"
The report also shows the major cost of operating a poison center is personnel: 76% of all costs. This expense is due to the 24/7 personnel-intense activity of handling public and health professional calls and the requirement for highly-trained expert staff.
Poison control centers lead to huge savings in the overall cost of our healthcare system. For every dollar spent on poison control, a series of studies conducted over the last two decades have shown cost savings of $6 to $36.3-14 One analysis pegs the return on investment at $13.39 per dollar spent (including medical care savings and reduced productivity loss), or $1.8 billion/year.2 These savings are attributed to 1) avoided medical utilization such as unnecessary ER visits ($752.9 million), reduced hospital length of stay due to poison control guidance ($441.1 million), prevention of poisonings ($23.9 million), and reduced work-loss days ($603 million).
Always in Crisis
A 1994 Congressional hearing1 shed light on the financial struggles of U.S. poison centers at the Federal level for the first time and led to the first coordinated Federal funding for U.S. poison control operations, although that funding covered only 12% to 15% of poison control costs. Across the U.S. both large and small poison centers were closing their doors and many of the surviving centers were struggling. But even then, two decades ago, the fact that poison centers were cost-effective and life-saving public health services was not disputed.
Unfortunately, two decades later, the financial exigencies have not abated. Federal funding for poison control was reauthorized in 2014 through the Poison Center Network Act (P.L. 113-77), authorizing the Federal funding of poison centers through FY 2019 at $30.1 million annually (the immediately prior authorizing legislation was P.L. 110-337, the Poison Center Support, Enhancement and Awareness Act of 2008). Most ($28.6M) of the authorized funding is designated for a grant program that funds operations of the 55 poison centers, awarded proportional to the population each center serves. A major contributor to the poison center funding problem stems from the fact that the Act is not funded at the authorized level. The Federal poison control program was funded at $29.3M in FY 2010, but in FY 2012 to FY 2015 appropriations were only at $18.8M of the authorized $30.1M. Thus poison centers nationally have experienced a 36% cut in Federal funding. Most centers have also experienced state and local funding cuts.
The Magnitude of the Poisoning Problem
Poisoning is now the leading cause of injury death in the U.S., surpassing motor vehicle traffic deaths. A dramatic increase in drug poisoning deaths, especially opioid deaths, is causing the rise. These fatalities result from both substance abuse and from therapeutic use of opioids.
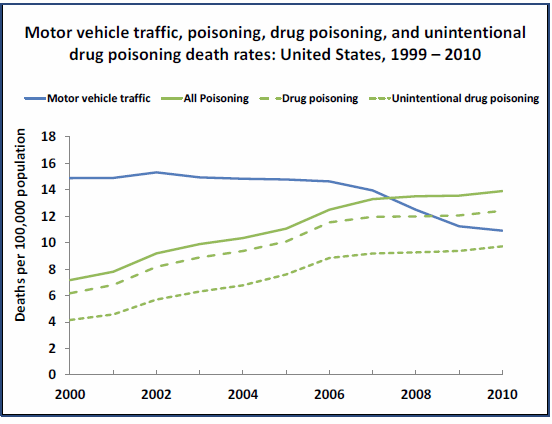
Note: "Drug Poisoning" is a subset of "all poisonings and includes unintentional, intentional,
and undetermined intents.
Source: National Vital Statistics System, 2000-2010
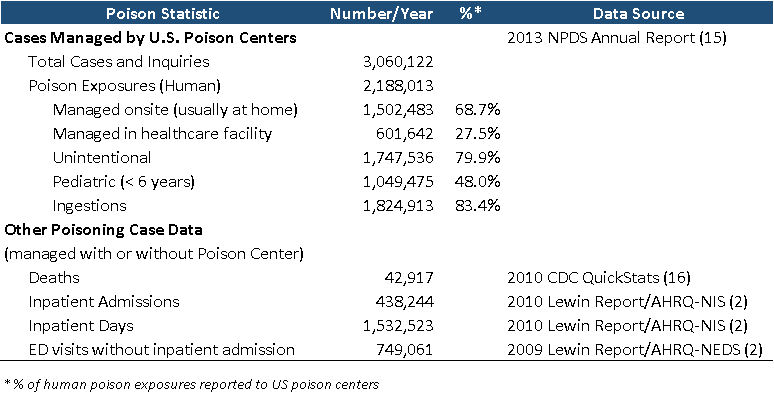
The table below incorporates poison control data from the National Poison Data System (AAPCC’s NPDS) and other data sources (CDC, AHRQ, NCHS) to provide a composite view of the extent of the poisoning problem in the U.S. By drawing from several data sources, it highlights the data from multiple perspectives, including cases reported to poison centers as well as deaths, hospital admissions and ED visits reported through other national databases.
Characterizing Calls to U.S. Poison Centers
The 55 US. Poison centers handle about 2.2 million human exposure cases annually. In 2013, U.S. poison centers handled 3,060,122 cases (8,384/day) including 2,188,013 human exposures (5,995/day), 59,496 animal exposures, 806,347 information calls (ranging from pill IDs [half of the info calls] to drug and poison questions), 6,116 human confirmed non-exposures (e.g. thought child took the pills, but later found them), and 150 animal confirmed non-exposures. Poison centers also place follow-up calls to provide additional information as the clinical course progresses, monitor outcomes, and provide poison prevention education. These follow-ups may increase the safety of guiding patients by phone. In 2013, 2,515,811 follow-up calls were placed, including at least one follow-up in 46.1% of human poison exposure cases and multiple follow-up calls (up to 121 calls) in 24.1% of cases.
Of the human poison exposures reported to U.S. poison centers in 2013, 48% involved children younger than 6 years, 6% involved youth 6-12 years of age, 7% involved teens, and 38% involved adults (>19 years). Peak poisoning frequency is in 1 and 2-year-old children, but no age group is immune.
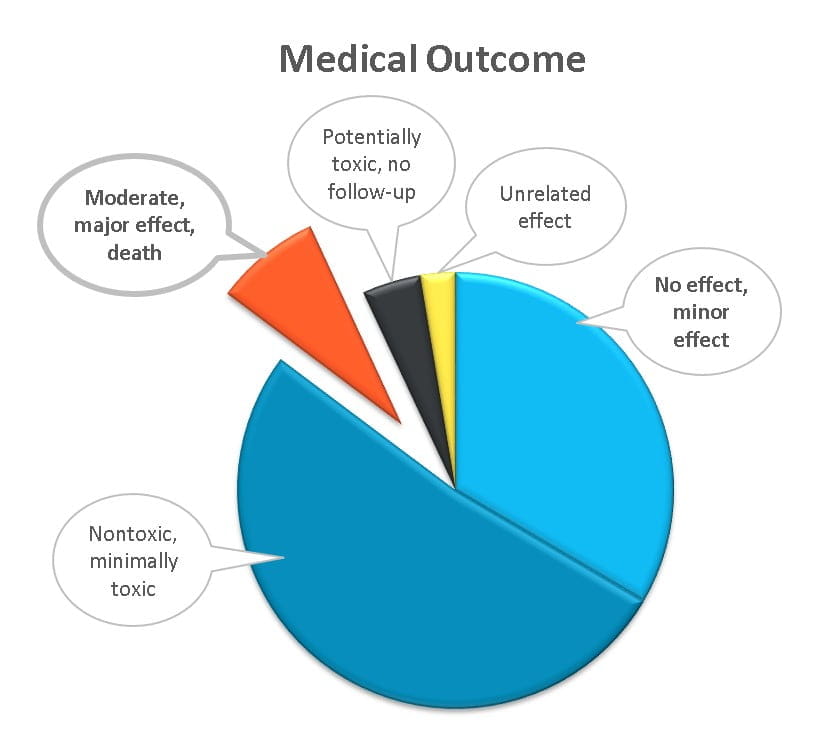
Most reported poison exposures are unintentional (80%, including therapeutic errors, bites and stings, occupational exposures, food poisoning, and “grazing” toddlers). Suicidal cases comprise 10.5% of reports, and are often more serious, involving larger quantities and/or more toxic substances. Poison centers also handle substance abuse, adverse reactions, tampering, and withdrawal cases.
The majority of cases reported to poison centers (69%) are managed on-site (usually at home) without health care intervention. About 28% of cases were managed in a healthcare facility (2013 NPDS data) with the guidance of a poison center. In most of these healthcare facility cases (79%; 2014 preliminary NPDS data), the patient was already in an ER or hospital when the poison center was called by the physician or other health professional for help managing the case. In the other 21% of the healthcare facility cases, the patient was referred in to a healthcare facility (ER usually) by Poison Control. Poison center cases have become more serious over time, with a 27% rise in the number of cases managed in a health care facility from 2000 to 2013.
Staffing U.S. Poison Centers
Physicians and other health professionals also rely on poison centers for their specialized toxicology expertise and generate about a quarter of the calls to Poison Control. That expertise is developed through training and certification programs for the nurses and pharmacist who provide the phone consultations (Certified Specialists in Poison Information) and for the clinical and medical toxicologists who provide backup, guidelines, training, surveillance, preparedness and research.
U.S. poison centers are staffed by Certified Specialists in Poison Information (CSPIs). These are specially trained registered nurses or pharmacists who sit for a national certifying exam after extensive on-the-job training in a poison center, and are eligible to take the exam after 2000 hours of experience and after handling a minimum of 2000 human poison exposure cases. Each trained and certified full-time Specialist handles about 3000 to 4000 human poison exposure cases annually.
Within each poison center there is also a mixture of board-certified medical toxicologists (physicians) and board-certified clinical toxicologists (American Board of Applied Toxicology [ABAT], mostly pursued by PharmDs although a small number of RNs and PhDs have achieved this board certification). Medical toxicologists (physicians) are most often trained initially in emergency medicine, then additionally trained in medical toxicology, although pediatricians, internists and occupational medicine physicians may also become medical toxicologists. There are about 600 board-certified medical toxicologists in the U.S. (not all practicing medical toxicology) and about 100-110 clinical toxicologists in the U.S. who are board-certified by the ABAT.
Surveillance
The real time collection of data by U.S. poison centers and its upload to AAPCC’s National Poison Data System (NPDS) every 8 minutes enables powerful monitoring of data to detect chemical/bioterrorism events, public health issues, product hazards, and emerging substance abuse problems. This surveillance is conducted at both the poison center level and the national level. It includes automated analyses around the clock for 1) hourly volume outliers, 2) outliers in any of 131 coded clinical effects occurring within the prior 24 hours, and 3) combinations of clinical effects suggestive of chemical/bioterrorism (anthrax, cyanide, botulism, nerve agents, blister agents, smallpox, etc). Email alerts go to toxicologists when outliers are detected, then further case analysis is performed to identify public health issues.
Poison centers have also established a strong track record of identifying product hazards and alerting regulators to these hazards. Examples include sounding the alarm for the 20 mm lithium coin cell causing esophageal perforations and deaths in toddlers. Poison centers have also urged reformulation, banning, label changes or repackaging for dibucaine-containing topicals, acetonitrile-containing nail glue removers, iron supplements, laundry detergent pods, lamp oil, and amoxapine (the antidepressant) – to name a few hazards we’ve detected and worked to eliminate. The synthetic marijuana “epidemic” and bath salts issues all received federal and media attention because of alerts from poison center data.
webPOISONCONTROL
U.S.poison centers have traditionally relied on the telephone to provide consultations - urging the public to call instead of guessing what to do in a poison emergency. However, over the past decade, more and more people have begun to turn to the internet for health information. At the end of 2014, the National Capital Poison Center launched an online triage app for poison emergencies - webPOISONCONTROL®. The app was developed to provide accurate triage guidance and a trusted resource for poison emergencies involving unintentionally swallowed substances, to replace the misinformation found elsewhere on the web. The pilot phase demonstrated that webPOISONCONTROL is a safe and reliable source of information for those who prefer the internet over the telephone. This triage app has the potential to:- Expand access to poison control services,
- Decrease the cost of managing poison emergency consults by replacing personnel-intensive telephone consultations with computer-guided recommendations, and
- Harmonize triage guidelines throughout U.S. poison centers.
At present, eight poison centers are participating in the webPOISONCONTROL project. Use webPOISONCONTROL for unintentionally swallowed poisons - taken once, by a human (not your dog). The app is for cases where symptoms haven’t developed yet, in people who are healthy, not pregnant, and between the ages of 6 months and 79 years.
References
- American Association of Poison Control Centers statement in “Hearing before the Human Resources and Intergovernmental Relations Subcommittee of the Committee on Government Operations”. House of Representatives. 103rd Congress, 2nd Session. Mar 15, 1994. P72-113.
- The Lewin Group. Value of the Poison Center System. Final Report. Sept 26, 2012.
- Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C, Sheppard M. The impact of poison control centers on poisoning-related visits to EDs--United States, 2003. Am J Emerg Med 2008; 26(3):310-315.
- Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C, Sheppard M. The potential impact of poison control centers on rural hospitalization rates for poisoning. Pediatrics 2006; 118(5): 2094-2100.
- Miller TR, Lestina DC. Costs of poisoning in the United States and savings from poison control centers: a benefit-cost analysis. Ann Emerg Med 1997; 29:239-245.
- Vassilev ZP, Marcus SM. The impact of a poison control center on the length of hospital stay for patients with poisoning. J Toxicol Environ Health: Part A 2007; 70(2):107-110.
- Bunn TL, Slavova S, Spiller HA, Colvin J, Bathke A, Nicholson VJ. The effect of poison control center consultation on accidental poisoning inpatient hospitalizations with preexisting medical conditions. J Toxicol Environ Health A 2008; 71:283-288
- King WD, Palmisano PA. Poison control centers: can their value be measured? South Med J 1991 Jun; 84(6):722-726.
- LoVecchio F, Curry S, Waszolek K, Klemens J, Hovseth K, Glogan D. Poison control centers decrease emergency healthcare utilization costs. J Med Toxicol 2008; 4(4):221-224.
- Phillips KA, Homan RK, Hiatt PH, Luft HS, Kearney TE, Heard SE, Olson K. The costs and outcomes of restricting public access to poison control centers: results from a natural experiment. Med Care 1998; 36(3):271-80.
- Harrison DL, Draugalis JR, Slack MK, Langley PC. Cost-effectiveness of regional poison control centers. Arch Intern Med 1996; 156(22):2601-2608.
- Blizzard JC, Michels JE, Richardson WH, Reeder CE, Schulz RM, Holstege CP. Cost-benefit analysis of a regional poison center. Clin Toxicol (Phila) 2008; 46(5):450-456.
- Hilton J, Wahl M. Poison centers and medical cost avoidance: Revisiting the concept $7 saved for every $ spent. Clin Toxicol (abstract) 2008; 46(7):591.
- Galvão TF, Silva MT, Silva CD, Barotto AM, Gavioli IL, Bucaretchi F, Atallah AN. Impact of a poison control center on the length of hospital stay of poisoned patients: retrospective cohort. Sao Paulo Med J 2011; 129(1):23-9.
- Mowry JB, Spyker DA, Cantilena LR Jr, McMillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014; 52(10):1032-283.
- CDC QuickStats: Number of deaths from poisoning, drug poisoning and drug poisoning involving opioid analgesics - United States, 1999-2010. MMRW 2013; 62(12):234.
Press Box
Press Release September 20, 2017
Poisoned? Get Expert Help.
Don't guess what you should do. Get accurate Poison Control answers online or by phone. Both are free and confidential.
or CALL 1-800-222-1222
Get the App!
Download the freewebPOISONCONTROL® app.
Subscribe to The Poison Post®
The Poison Post® is a free, quarterly e-newsletter delivering poison prevention tips right to your inbox!
Poison Statistics
Support Us
webPOISONCONTROL® is funded entirely through generous private contributions. Your donation to our 501(c)(3) charitable organization will help us maintain and expand this free service so that others can get life-saving help for poison exposures.


